Revenue Cycle Management
Managing the full revenue cycle from claims processing to revenue payments requires a team of highly skilled, experienced, and tech-savvy professionals. We realize that in this new era of declining reimbursements and the shift towards higher copays and deductibles has changed the rules of revenue cycle management. Partnering with TAK will ensure your practice revenue collections process overcomes these challenges.
Our team works closely with you and your staff to customize and implement front-end office processes for claim payment optimization. On the back-end, our staff employs a comprehensive Revenue Cycle Management strategy that reduces the time required for claim resolution and maximizes revenue payments.
TAK customizes real-time reports, showing trends, and benchmarking productivity against national and specialty specific standards. Our goal is to surpass all standards while helping you achieve your financial objectives.
We have great confidence in our Claims Department’s abilities. Our Claims Specialists are recognized on an industry level for consistently achieving a claim rate of 97% to 99% of claims being paid on the first submission.
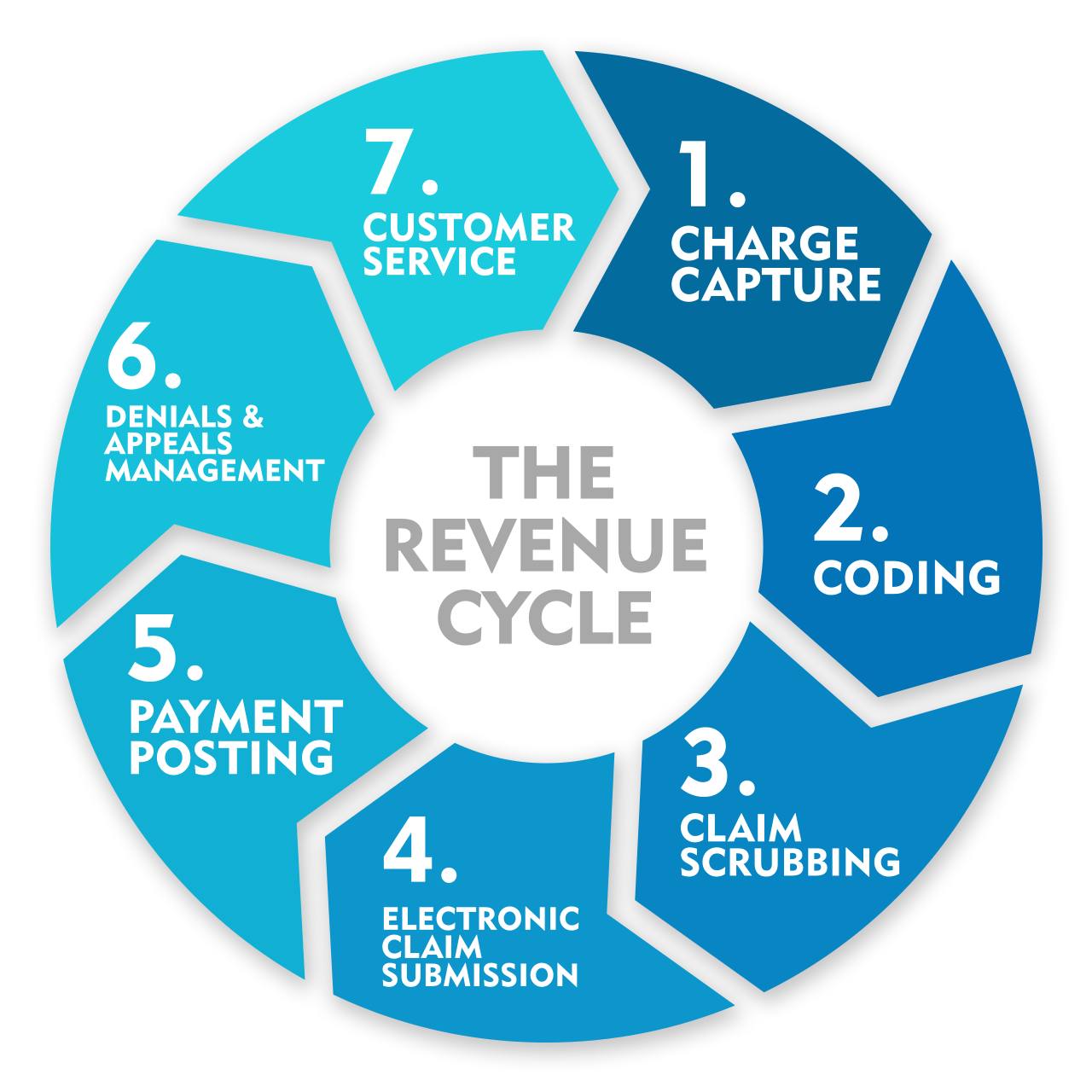
The revenue cycle begins on the front-end with patient scheduling, registration, demographics, insurance verification and eligibility, prior authorizations, referrals, and the collection of co-pays and deductibles. On the back-end, TAK provides the following RCM Services:
Billing
- Eligibility and Benefit Verification
- Authorization Request and Tracking
- Charge Capture
- Coding Correction and Reimbursement Maximization
- Claim Scrubbing
- Electronic Insurance Claim Submission
- Claims follow up
- Denials Review and Appeals Management
- Appeal of all Denied or Low Paid Claims
Payment Processing
- Posting of Insurance and Patient Payments
- Cash/Checks Postings and Daily Bank Deposits
- Credit Card Merchant Services and Management
Accounts Receivables
- Patient Billing, Statement Processing and Mailing
- Incoming Patient Calls and Outreach
- Automated Collection and Telephone Follow-ups
- A/R Collections
Administration
- Practice Staff Training and Ongoing Support
- HIPAA Compliance
- Fee Schedule Review and Analysis
Monthly Revenue Cycle Management Reports
- Revenue Cycle Management Analysis
- Provider Patient Data and Revenue Reporting vs Contract Requirements
- Accounts Receivable Aging Report
- Patient Mix and CPT Code Reports
- Insurance Reimbursement Reports
- Unpaid Claims Analysis
- Missed Appointments, Cancellations & No Shows
- Practice Management Analysis, Tools and Reports
Contact Us
Office: 978-227-5730
Email: paghassi@takmedgroup.com
Address:
14 Monument Square
Leominster, MA 01453
2017 TAK MEDICAL GROUP. ALL RIGHTS RESERVED








